By Tom Hagy
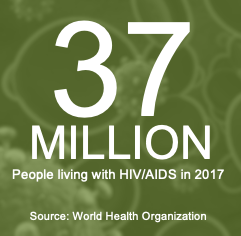 I worked in the press office of the New Jersey Department of Health in the 1980s. Aside from hazardous waste, asbestos, cancer, a chemical fire or two, the annual influenza “crisis” and the occasional salmonella outbreak, AIDS was one of the most urgent, frightening and misunderstood health issues of the day. The U.S. epidemic began with one reported case in 1981, according to the Centers for Disease Control, and grew to an astounding 36.9 million people living with HIV/AIDS in 2017 as reported by the World Health Organization.
I worked in the press office of the New Jersey Department of Health in the 1980s. Aside from hazardous waste, asbestos, cancer, a chemical fire or two, the annual influenza “crisis” and the occasional salmonella outbreak, AIDS was one of the most urgent, frightening and misunderstood health issues of the day. The U.S. epidemic began with one reported case in 1981, according to the Centers for Disease Control, and grew to an astounding 36.9 million people living with HIV/AIDS in 2017 as reported by the World Health Organization.
The office I worked in was tasked with providing information to the public and members of the press. At the time many public health professionals believed — as is the case with many diseases — that education on how to prevent transmission of the HIV virus would all but eliminate its spread. All we had to do was educate the public and, most importantly, the high-risk groups. Education is a common weapon in fighting disease. It’s why we wash our hands, cough into our elbows and try not to put salt on absolutely everything we put in our mouths.
In the early 1980s the “problem” was that the high-risk groups were having homosexual sex and injecting drugs — not typical themes addressed by politicians. Early on more conservative policymakers didn’t want to distribute pamphlets on methods of having safe homosexual sex — such as mutual masturbation and condom use during anal sex — or exercising hygienic methods of shooting heroin. (The state, did, however, have a needle-exchange program to keep addicts from re-using syringes.)
I recall the frustration of at least one of the state’s public health professionals and AIDS awareness groups who strongly advocated for education — and the more specific the better. The political reality — that the state could at least slow down the epidemic through education but policymakers were not anxious to put their names on “how to” guides for gay sex and illegal drug use — troubled me. At first I didn’t understand it. Then I did. And yet again, I really didn’t. What about our mission of ensuring public health and safety? Well, gradually public health physicians prevailed and policymakers got it. If you look at the NJ DOH website today you will find all kinds of information on prevention and treatment of the disease. They offer HIV Care and Support Services and educational events. They continue to have a syringe access program with listings of locations where drug users can safely dispose of dirty injection equipment and walk away with clean syringes and needles.
AIDS would go on to claim the lives of 448,000 people in the U.S. by the end of 2000. Thanks to medical advancements — and educational programs and services offered by non-governmental and governmental organizations, like the NJ DOH — the rate of deaths slowed. Still, in 2017, 940,000 people died from HIV-related illnesses worldwide, according to WHO.
The social stigma of homosexuality and, relevant to this post, drug use, most certainly played a role in allowing the disease to spread. The same is true today when it comes to the opioid crisis. According to the Hazelden Betty Ford Foundation website there are insufficient resources dedicated to confronting addiction due in part to public stigma.
A Moral Issue or a Health Problem?
 “For generations, [the] combination of personal shame and public stigma has produced tremendous obstacles to addressing the problem of alcoholism and other drug addiction in America. Today, the stigma of addiction is seen as a primary barrier to effective addiction prevention, treatment and recovery efforts at the individual, family, community and societal levels,” the Hazelden Betty Ford Foundation site reads. “Addiction stigma prevents too many people from getting the help they need. Drug and alcohol addiction is too often seen as a moral issue or a criminal matter rather than a health problem. Many public policies and practices related to housing, education, jobs, voting rights and insurance discriminate against individuals who have addiction, even after they’ve established long-term recovery.”
“For generations, [the] combination of personal shame and public stigma has produced tremendous obstacles to addressing the problem of alcoholism and other drug addiction in America. Today, the stigma of addiction is seen as a primary barrier to effective addiction prevention, treatment and recovery efforts at the individual, family, community and societal levels,” the Hazelden Betty Ford Foundation site reads. “Addiction stigma prevents too many people from getting the help they need. Drug and alcohol addiction is too often seen as a moral issue or a criminal matter rather than a health problem. Many public policies and practices related to housing, education, jobs, voting rights and insurance discriminate against individuals who have addiction, even after they’ve established long-term recovery.”
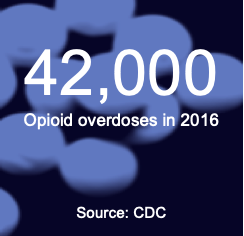
The CDC reported that in 2016 there were 63,600 drug overdoses — a jump of 21% in one year. Opioids are currently the main driver of drug overdoses, comprising 42,000 of the annual total. The states of Ohio, West Virginia, New Hampshire, Washington, DC and Pennsylvania see the most opioid overdoses.
As reported by NPR last year, the crisis has reversed the trend of lengthening life expectancies which fell two years in a row. It was 78.9 in 2014; in 2016 it fell to 78.6. The last time it fell was in 1993 due to the AIDS epidemic, but hasn’t fallen two years in a row since the 1960s, NPR reported based on government statistics.
The Monetary Cost
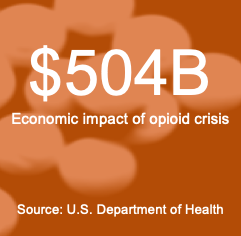
In addition to the toll on life and health, the opioid crisis is costly. The U.S. Department of Health puts the economic costs at $504 billion, which includes healthcare costs, criminal justice costs, lost productivity due to addiction and incarceration, and more. The CDC puts the annual cost of the opioid crisis at $75 billion.
 Efforts to recover these costs include litigation. From there, defendants turn to the insurers where another layer of dispute arises.
Efforts to recover these costs include litigation. From there, defendants turn to the insurers where another layer of dispute arises.
Speaking on an HB webinar titled Insurance Coverage Issues Arising from Opioid Litigation and Investigations, policyholder attorney Bernard Bell of Miller Friel PLLC said lawsuits fall into three categories: 1) state and local governments, and tribes, are suing to recover expenses associated with their response to opioid abuse; 2) suits against manufacturers for alleged gross misrepresentation of the risks and against distributors for failing to monitor suspicious orders; and 3) individuals suing drug makers and distributors for their addictions.
There are 2,000 lawsuits pending, with 1,200 of them in MDL in the U.S. District Court for the Northern District of Ohio in Cleveland. Plaintiff attorneys have recently said that a mandatory class maybe be the only way to resolve the litigation.
A new class action lawsuit filed in November 2018 in West Virginia seeks to represent children exposed to opioids in utero. According to Top Class Actions, the suit alleges that in 2017, 50 out of every 1,000 babies born in West Virginia were born addicted to opioids.
Many of the costs associated with the crisis “don’t always fit very well with specific losses that insurance policies are designed to cover,” said insurance industry attorney Laura Foggan of Crowell & Moring LLP.
For that reason, and with so much at stake, so much liability, and so many deep pockets, we can expect policyholders and insurers to battle the issue out in the courts.
Foggan and Bell addressed the insurance aspects of the litigation during a recent HB webinar, titled Insurance Coverage Issues Arising from Opioid Litigation and Investigations. The program is now available on-demand. Click to register.
